This article is for informational purposes only and is not a substitute for medical advice. Please consult a licensed dermatologist for personalized care.” — adds legal clarity and aligns with best practices.
Acne is one of the most common skin conditions affecting people of all ages, not just teenagers. For many, it appears as mild pimples or blackheads. However, in more severe cases, acne can develop into cysts or nodules—painful, deep lesions that require medical attention. Understanding when to consult a dermatologist is essential for effective treatment and long-term skin health.

Understanding Cystic and Nodular Acne
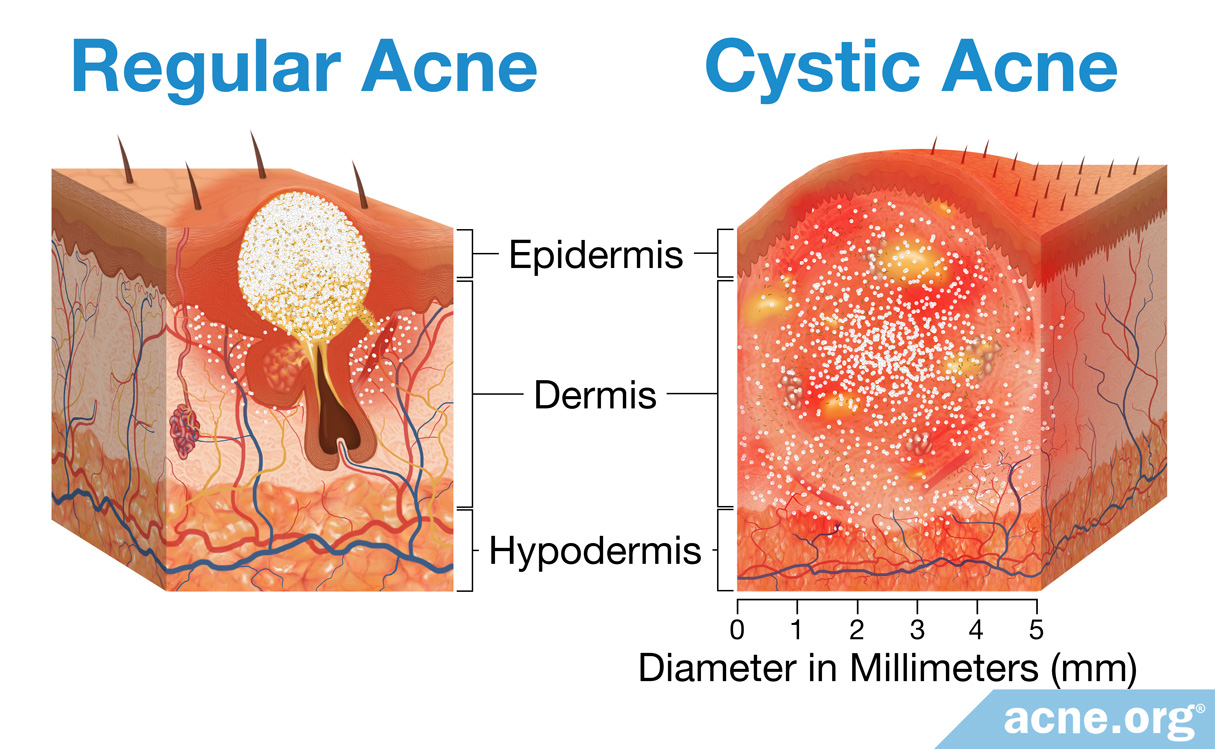
Cystic acne and nodular acne are severe forms of acne vulgaris. According to the American Academy of Dermatology (AAD), these types of acne develop when pores in the skin become clogged with oil, dead skin cells, and bacteria. The inflammation penetrates deeper into the skin than typical pimples, leading to large, tender lumps beneath the surface.

Cysts vs. Nodules
-
Cysts are pus-filled lumps that resemble boils and can rupture, potentially leading to scarring.
-
Nodules are hard, painful bumps that form deep within the skin but typically do not contain pus.
Both conditions can appear on the face, back, shoulders, and upper arms and often persist for weeks or longer without treatment.
Signs It’s Time to See a Dermatologist
Dermatologists are medical doctors who specialize in diagnosing and treating skin conditions. While mild acne can often be managed with over-the-counter products, more severe or persistent forms require professional care. Here are key indicators that you should consult a dermatologist:
1. You Have Painful, Deep Lesions
If you’re experiencing large, painful cysts or nodules that don’t go away or recur frequently, it’s time to seek medical advice. These types of lesions are unlikely to respond to topical drugstore treatments and carry a higher risk of causing permanent scarring.
2. Your Acne Is Persistent or Worsening
Some people deal with persistent acne, which starts in adolescence and continues into adulthood. Others develop late-onset acne, which appears for the first time in their 20s, 30s, or even later. In both cases, seeing a dermatologist can help uncover underlying causes such as hormonal imbalances or chronic inflammation.
According to the National Institutes of Health (NIH), persistent acne may indicate deeper dermatological or systemic conditions, including polycystic ovary syndrome (PCOS), which should be properly evaluated by a healthcare provider.

3. You’re Experiencing Emotional Distress
Severe acne can take a toll on mental well-being. Research published in the Journal of the American Academy of Dermatology indicates that acne can lead to low self-esteem, social withdrawal, and even depression. If your skin condition is affecting your quality of life, professional treatment can make a significant difference.

4. Over-the-Counter Products Aren’t Working
If you’ve been using non-prescription products containing ingredients like benzoyl peroxide or salicylic acid for several weeks without improvement, a dermatologist can prescribe more potent treatments. These may include:
-
Topical retinoids
-
Antibiotics
-
Hormonal therapies
-
Oral isotretinoin (Accutane), for the most severe cases
5. You Notice Scarring or Skin Discoloration
Early intervention is key to preventing acne scarring. Dermatologists can provide options such as corticosteroid injections, chemical peels, or laser therapy to reduce the risk of permanent marks.

Common Causes of Adult Acne
Understanding the triggers behind acne can help guide treatment. Common causes include:
-
Hormonal changes: Fluctuations during menstruation, pregnancy, or menopause can lead to increased oil production.
-
Stress: Elevated stress levels can exacerbate acne by increasing androgen hormone production.
-
Diet: While more research is needed, some studies suggest that high-glycemic foods and dairy may aggravate acne in certain individuals.
-
Genetics: A family history of acne increases the likelihood of experiencing it.
-
Cosmetic products: Using non-comedogenic (non-pore-clogging) products is essential for acne-prone skin.
Effective Treatments Offered by Dermatologists
Dermatologists tailor acne treatment plans to the individual’s skin type, age, and severity of the condition. These may include:
Prescription Medications
-
Topical treatments: Including retinoids and antibiotics to reduce bacteria and inflammation.
-
Oral medications: Such as antibiotics, hormonal treatments like birth control pills, or spironolactone for women with hormonal acne.
-
Isotretinoin: A powerful retinoid for severe cystic acne that hasn’t responded to other treatments. It requires careful monitoring due to potential side effects.
In-Office Procedures
-
Cortisone injections: For immediate relief of painful nodules or cysts.
-
Drainage and extraction: In rare cases, dermatologists may safely drain large cysts under sterile conditions. This should never be attempted at home, as improper handling can lead to infection or scarring.
-
Chemical peels and laser therapy: Used to improve skin texture, reduce inflammation, and minimize scarring.
Prevention and Maintenance Tips
Once acne is under control, ongoing care is important to maintain clear skin and avoid future breakouts. The AAD recommends:
-
Gentle cleansing: Use a mild cleanser twice daily and avoid scrubbing.
-
Moisturizing: Even acne-prone skin needs hydration. Choose oil-free, non-comedogenic moisturizers.
-
Sun protection: Use a broad-spectrum SPF 30+ sunscreen daily to protect your skin and prevent post-inflammatory hyperpigmentation.
-
Consistent routine: Give treatments time to work—many take 6–8 weeks to show results.
Conclusion
Severe acne in the form of cysts or nodules is a medical condition that deserves proper care. Whether your acne has persisted from adolescence or has recently appeared for the first time in adulthood, a board-certified dermatologist can provide a comprehensive treatment plan tailored to your needs.
Consulting a professional not only helps alleviate physical symptoms but also supports your emotional well-being and confidence. Don’t wait for painful lesions or scars to develop—early intervention can make all the difference.
Sources:
-
American Academy of Dermatology Association (AAD): www.aad.org
-
National Institutes of Health (NIH): www.nih.gov
-
Journal of the American Academy of Dermatology
-
Mayo Clinic: www.mayoclinic.org





